Smell (olfaction) disorders
Understanding Smell (Olfaction) Disorders
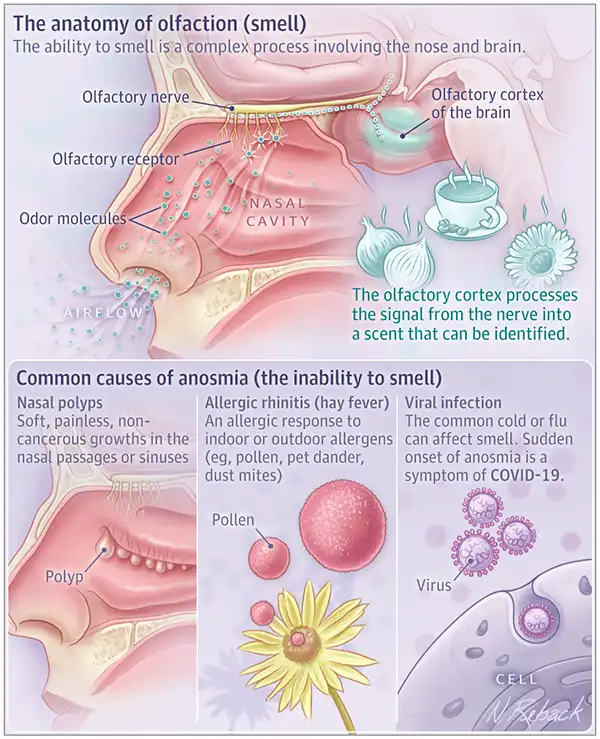
The sense of smell, or olfaction, is a complex chemosensory system crucial for detecting airborne odorant molecules (odorivectors). Disorders of olfaction can significantly impact an individual's quality of life, affecting taste perception, appetite, detection of environmental hazards (e.g., smoke, gas leaks), and social interactions.
Types of Olfactory Dysfunction
Olfactory disorders are broadly categorized based on the nature of the dysfunction:
- Hyposmia: A decreased or reduced ability to smell.
- Anosmia: The complete absence or loss of the sense of smell.
- Hyperosmia: An abnormally increased or heightened sensitivity to odors.
- Parosmia: A distorted or perverted sense of smell, where familiar odors are perceived differently, often unpleasantly (e.g., a pleasant smell is perceived as foul). This is sometimes referred to as troposmia.
- Cacosmia: A specific type of parosmia where odors are perceived as foul or disgusting. Sometimes also used to describe the perception of a foul odor when no odor is actually present (olfactory hallucination or phantosmia).
- Phantosmia: The perception of an odor when no odorant is actually present (olfactory hallucination).
- Agnosmia: Inability to classify or verbally describe an odor, despite being able to detect its presence.
Causes of Olfactory Disorders: Conductive vs. Sensorineural
Olfactory disorders can be broadly classified based on the location of the problem within the olfactory pathway:
- Conductive (Transport or Respiratory) Olfactory Loss: This occurs when odorant molecules are physically prevented from reaching the olfactory neuroepithelium, which is located high in the nasal cavity within the olfactory cleft. Common causes include:
- Nasal Polyps: Benign growths in the nasal cavity that can block airflow to the olfactory region.
- Deviated Nasal Septum: Particularly high septal deviations that narrow or obstruct the olfactory cleft.
- Mucosal Inflammation and Swelling: Due to acute or chronic rhinitis (viral, bacterial, allergic), sinusitis, or other inflammatory conditions.
- Nasal Tumors: Benign or malignant neoplasms obstructing the nasal passages.
- Chronic Hypertrophic Rhinitis: Enlarged turbinates blocking airflow.
- Nasal Synechiae or Atresia: Scar tissue adhesions or congenital blockages.
- Sensorineural Olfactory Loss (Essential Anosmia/Hyposmia): This results from damage to the olfactory neuroepithelium itself, the olfactory nerve (cranial nerve I), or the central olfactory pathways in the brain (olfactory bulb, tract, cortex). Causes include:
- Viral Infections: Upper respiratory tract infections, particularly influenza-like illnesses, are a common cause of post-viral olfactory dysfunction (PVOD) due to direct damage to olfactory receptor neurons.
- Ozena (Atrophic Rhinitis): Severe atrophy of the nasal mucosa, including the olfactory epithelium.
- Head Trauma: Can shear or damage olfactory nerve filaments as they pass through the cribriform plate, or cause contusion to olfactory brain regions.
- Neurodegenerative Diseases: Parkinson's disease, Alzheimer's disease often present with early olfactory loss.
- Toxins and Medications: Exposure to certain chemicals, heavy metals, or side effects of some medications.
- Congenital Anosmia/Hyposmia: Present from birth (e.g., Kallmann syndrome).
- Intracranial Tumors or Lesions: Affecting the olfactory pathways (e.g., meningiomas of the olfactory groove).
- Aging (Presbyosmia): Natural decline in olfactory function with age.
- Systemic Diseases: Conditions like hypothyroidism, diabetes, vitamin deficiencies (e.g., B12).
Progression of Olfactory Loss
Conductive (respiratory) hyposmia or anosmia can sometimes transition into a sensorineural (essential) form if the underlying cause is not addressed and leads to chronic inflammation or damage to the olfactory epithelium. Initially, the impairment of smell might be unstable, with periods of partial recovery. However, as the disease progresses (e.g., chronic inflammation, polyp growth), the hyposmia can become constant and eventually evolve into essential anosmia due to degeneration of the peripheral receptors of the olfactory analyzer. It's important to recognize that virtually any pathology causing significant nasal obstruction can affect the sense of smell to some extent, as the olfactory receptor apparatus is located directly within the nasal cavity. However, hyposmia and anosmia can also occur even with apparently free nasal breathing if there is a subtle obstruction specifically affecting the olfactory cleft (e.g., small polyps in the olfactory area, localized swelling closing the olfactory gap). In all such cases, the primary issue is the disturbed contact between odoriferous substances and the olfactory receptors.
Diagnosis of Smell (Olfaction) Disorders
Clinical Evaluation and Diagnostic Tests
The diagnosis of smell disorders involves a comprehensive approach:
- Detailed Medical History: Inquiring about the onset (sudden or gradual), duration, nature (e.g., reduced smell, distorted smell, phantom smells), severity of the olfactory disturbance, any preceding events (URI, head trauma, toxin exposure), associated nasal symptoms (congestion, discharge), medical history (allergies, sinus disease, neurological conditions), medications, and smoking habits.
- Physical Examination:
- Rhinoscopy and Nasal Endoscopy: Thorough examination of the nasal cavities using anterior rhinoscopy and, more importantly, nasal endoscopy (micro-rhinoscopy) to identify any anatomical abnormalities (deviated septum, polyps, tumors), signs of inflammation (rhinitis, sinusitis), mucosal swelling, or obstruction of the olfactory cleft.
- Olfactory Function Testing (Olfactometry):
- Qualitative Tests: Involve identifying common odors presented to each nostril separately (e.g., coffee, peppermint, soap).
- Quantitative Tests: Measure odor detection thresholds (the lowest concentration of an odorant that can be perceived) and odor identification ability using standardized psychophysical tests like the University of Pennsylvania Smell Identification Test (UPSIT), Sniffin' Sticks, or Connecticut Chemosensory Clinical Research Center (CCCRC) test. These provide a more objective measure of olfactory function.
- Adrenaline (Epinephrine) or Ephedrine Test: This test helps differentiate between conductive (respiratory) and sensorineural (essential) hyposmia or anosmia. The nasal mucous membrane, particularly around the olfactory cleft, is lubricated (anemized) with a 0.1% epinephrine solution or a 3% ephedrine solution. This shrinks the mucosa, potentially opening up the olfactory cleft.
- If the sense of smell significantly improves after anemization, it suggests a **conductive olfactory loss** (the olfactory receptors are intact, but odorants were not reaching them).
- If there is no change in the sense of smell, it points towards a **sensorineural olfactory loss** (damage to the olfactory receptors, nerve, or central pathways).
- If there is some, but not complete, improvement, it may indicate a **mixed conductive and sensorineural loss**.
- Imaging Studies:
- CT Scan of the Paranasal Sinuses: Useful for evaluating inflammatory sinonasal disease, polyps, tumors, or anatomical obstructions.
- MRI of the Brain and Olfactory Pathways: May be indicated if a central cause (e.g., intracranial tumor, olfactory bulb/tract lesion, neurodegenerative disease) is suspected, especially with sudden onset anosmia without clear nasal pathology or associated neurological symptoms.
- Neurological Examination: If a central cause is suspected.
- Allergy Testing: If allergic rhinitis is a potential contributing factor.
Treatment Approaches for Smell (Olfaction) Disorders
The treatment of olfactory disorders depends heavily on the underlying cause and the type of dysfunction.
Treating Conductive Olfactory Loss
If the olfactory loss is conductive, treatment is aimed at addressing the physical obstruction preventing odorants from reaching the olfactory epithelium. This often involves:
- Medical Management of Inflammatory Conditions:
- Treating chronic rhinitis or sinusitis with nasal saline irrigations, intranasal corticosteroids, antibiotics (if bacterial infection is present), or oral corticosteroids for severe inflammation or polyps.
- Managing allergic rhinitis with antihistamines, intranasal corticosteroids, and allergen avoidance or immunotherapy.
- Surgical Interventions: Microsurgical techniques, often performed endoscopically with surgical optics (microscope or endoscope), are employed to correct anatomical obstructions:
- Polypectomy: Removal of nasal polyps.
- Septoplasty: Correction of a significantly deviated nasal septum, especially if it obstructs the olfactory cleft.
- Turbinate Reduction: For chronic hypertrophic rhinitis.
- Functional Endoscopic Sinus Surgery (FESS): To open blocked sinus pathways and remove diseased tissue in chronic rhinosinusitis.
- Repair of Synechiae or Atresia.
- Management of Nasal Injuries.
- Excision of Nasal Tumors.
Managing Sensorineural Olfactory Loss
Treatment for sensorineural olfactory loss is often more challenging, as it involves damage to the olfactory receptors or neural pathways. Options include:
- Addressing the Underlying Cause: If a specific cause is identified (e.g., treating a systemic disease, discontinuing an offending medication, managing a neurological condition), this may sometimes lead to partial recovery.
- Corticosteroids: Systemic or topical corticosteroids may be tried, particularly for post-viral olfactory dysfunction or inflammatory causes, as they can reduce inflammation that might be affecting olfactory neurons. Their efficacy is variable.
- Olfactory Training (Smell Training): Involves regular, conscious sniffing of a set of specific odors (e.g., rose, eucalyptus, lemon, clove) for several months. This aims to stimulate and potentially regenerate olfactory pathways. It has shown some benefit, particularly in post-viral and post-traumatic olfactory loss.
- Vitamin Therapy: B-group vitamins (particularly B12) and other supplements (e.g., alpha-lipoic acid, zinc) have been suggested, but evidence for their efficacy is generally limited or inconsistent. Stimulating therapy might be prescribed.
- Investigational Therapies: Research is ongoing into other potential treatments, including nerve growth factors or stem cell therapies, but these are not yet standard clinical practice.
Unfortunately, for many cases of severe or long-standing sensorineural anosmia, especially post-traumatic or congenital, recovery may be limited or absent.
Addressing Hyperosmia and Parosmia/Cacosmia
- Hyperosmia: Treatment involves identifying and managing the underlying cause (e.g., neurological conditions like migraine, pregnancy, certain medications). Avoidance of trigger odors is key.
- Parosmia/Cacosmia: These often occur during the recovery phase of post-viral or post-traumatic olfactory loss. Management can be difficult. Olfactory training may sometimes help. In severe, persistent cases, counseling is important. Addressing any underlying sinonasal inflammation is also crucial. Treating the primary disease (e.g., neurasthenia, influenza) is fundamental.
Impact and Complications of Olfactory Disorders
Olfactory dysfunction can have a profound impact on an individual's life:
- Quality of Life: Reduced enjoyment of food (as much of flavor perception is smell-related), inability to appreciate pleasant aromas (flowers, perfumes).
- Safety Concerns: Inability to detect warning odors such as smoke from a fire, natural gas leaks, or spoiled food.
- Nutritional Issues: Anosmia can lead to decreased appetite, weight loss, or conversely, overconsumption of highly palatable (often unhealthy) foods to compensate for lack of flavor.
- Mood and Psychological Well-being: Olfactory loss has been linked to depression, anxiety, and social isolation.
- Occupational Hazards: For professions where a keen sense of smell is important (e.g., chefs, perfumers, firefighters).
Early diagnosis and management are important to mitigate these impacts where possible.
Differential Diagnosis of Olfactory Dysfunction
A comprehensive differential diagnosis is necessary when evaluating olfactory disorders:
| Category of Cause | Specific Examples | Typical Olfactory Presentation |
|---|---|---|
| Inflammatory/Obstructive Nasal & Sinus Disease | Chronic rhinosinusitis, nasal polyposis, allergic rhinitis, deviated septum, adenoid hypertrophy (in children) | Often conductive hyposmia/anosmia; may have parosmia. Usually improves with treatment of underlying nasal/sinus condition. |
| Post-Viral Olfactory Dysfunction (PVOD) | Following URI (e.g., influenza, common cold, COVID-19) | Often sudden onset of anosmia or severe hyposmia; parosmia common during recovery. Sensorineural. |
| Head Trauma | Fracture of cribriform plate, shearing of olfactory filaments, contusion of olfactory bulb/cortex | Often sudden and severe anosmia; can be permanent. Sensorineural. |
| Neurodegenerative Diseases | Alzheimer's disease, Parkinson's disease | Gradual onset hyposmia/anosmia, often an early symptom. Sensorineural. |
| Congenital Causes | Isolated congenital anosmia, Kallmann syndrome | Anosmia present from birth. Sensorineural. |
| Toxins/Medications | Exposure to certain industrial chemicals, heavy metals; side effects of some drugs (e.g., certain antibiotics, antihypertensives) | Variable onset and severity. Can be sensorineural. |
| Intracranial Tumors/Lesions | Meningioma of olfactory groove, frontal lobe tumors | Often unilateral anosmia initially, may progress; associated neurological signs. Sensorineural. |
| Aging (Presbyosmia) | Natural decline in olfactory neurons and function | Gradual decline in smell sensitivity. Sensorineural. |
| Psychiatric/Psychological Conditions | Depression, schizophrenia (can cause phantosmia or altered smell perception) | Often phantosmia or cacosmia. Requires psychiatric evaluation. |
When to Consult an ENT Specialist
Individuals should seek consultation with an Ear, Nose, and Throat (ENT) specialist for olfactory disorders if they experience:
- Sudden or unexplained loss or change in the sense of smell.
- Gradual but progressive decline in olfactory function.
- Distorted sense of smell (parosmia) or perception of phantom smells (phantosmia).
- Olfactory dysfunction accompanied by other nasal symptoms like persistent congestion, discharge, facial pain, or nosebleeds.
- Olfactory loss following a head injury or severe viral infection.
- Concerns about safety due to impaired smell (e.g., inability to detect gas or smoke).
- Significant impact on quality of life due to altered smell or taste.
An ENT specialist can perform a thorough evaluation, including nasal endoscopy and olfactory testing, to determine the cause of the smell disorder and recommend appropriate management strategies.
References
- Doty RL. Olfactory dysfunction. JAMA. 2018;319(4):408-409.
- Hummel T, Whitcroft KL, Andrews P, et al. Position paper on olfactory dysfunction. Rhinology. 2017 Mar 1;54(Suppl 26):1-30.
- Boesveldt S, Postma EM, Boak D, et al. Anosmia—A Clinical Review. Chem Senses. 2017 Sep 1;42(7):513-523.
- Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2016 Mar;6(3):299-307.
- Mann NM. Management of smell and taste disorders. Cleve Clin J Med. 2002 Jan;69(1):58-60, 63-4, 67-9.
- Kern RC. Chronic sinusitis and anosmia: a review. Int J Otorhinolaryngol. 2000 Aug;5(2):137-42.
- Snow JB Jr, Doty RL, Bartoshuk LM. Clinical evaluation of olfactory and gustatory disorders. In: Snow JB Jr, Ballenger JJ, eds. Ballenger's Otorhinolaryngology Head and Neck Surgery. 16th ed. BC Decker; 2003:chap 33.
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis