Nasal septal hematoma, nasal septal abscess
- Understanding Nasal Septal Hematoma and Abscess
- Symptoms and Clinical Presentation
- Diagnosis of Nasal Septal Hematoma and Abscess
- Treatment of Nasal Septal Hematoma and Abscess
- Potential Complications
- Differential Diagnosis of Bilateral Nasal Obstruction
- Prevention and When to Seek Urgent Care
- References
Understanding Nasal Septal Hematoma and Abscess
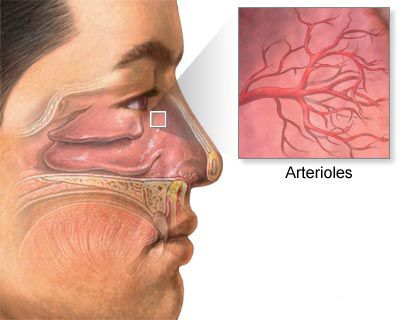
A nasal septal hematoma is a collection of blood within the space between the nasal septal cartilage (or bone) and its overlying perichondrium (for cartilage) or periosteum (for bone). If this hematoma becomes infected, it can progress to a nasal septal abscess, which is a collection of pus in the same subperichondrial or subperiosteal plane. Both conditions are considered otolaryngologic emergencies due to the potential for serious complications, including cartilage destruction and cosmetic deformity.
Pathophysiology: From Hematoma to Abscess
Following nasal trauma or other inciting events, blood vessels within the nasal septum can rupture. If the perichondrium is lifted away from the underlying cartilage by this bleeding, blood accumulates in this potential space, forming a hematoma. The nasal septal cartilage is avascular (lacks its own blood supply) and relies on diffusion of nutrients from the adherent perichondrium. When a hematoma separates these two layers, the cartilage is deprived of its blood supply, making it vulnerable to necrosis (tissue death) and infection. If bacteria, often from the nasal cavity itself, colonize the hematoma, it can transform into a septal abscess. This progression can occur rapidly, often within a few days.
Causes and Risk Factors
The most common causes and risk factors for nasal septal hematoma, and subsequently abscess, include:
- Nasal Trauma: This is the leading cause. Direct blows to the nose from falls, impacts during sports, altercations, or accidents can fracture the nasal bones or septal cartilage, leading to bleeding and hematoma formation. Even minor trauma without fracture can sometimes cause a hematoma.
- Nasal Surgery: Procedures involving the nasal septum, such as septoplasty or submucous resection, can occasionally lead to postoperative hematoma formation if bleeding occurs in the subperichondrial plane.
- Spontaneous Hematoma: Rarely, septal hematomas can occur spontaneously, particularly in individuals with bleeding disorders (e.g., hemophilia, von Willebrand disease) or those on anticoagulant therapy (e.g., warfarin, heparin, DOACs).
- Infectious Diseases: While less common as a primary cause, severe systemic infectious diseases like influenza, measles, or scarlet fever, or even severe local nasal infections, can theoretically predispose to septal mucosal friability and bleeding, potentially leading to a hematoma if other factors are present. However, trauma remains the predominant cause.
- Nose Picking or Foreign Bodies: Vigorous nose picking or insertion of foreign objects can traumatize the septal mucosa.
Infection of a pre-existing nasal septal hematoma is the primary cause of a septal abscess. The bacteria involved are often common nasal flora, such as *Staphylococcus aureus*, *Streptococcus pneumoniae*, and *Haemophilus influenzae*.
Symptoms and Clinical Presentation of Nasal Septal Hematoma and Abscess
The symptoms of nasal septal hematoma and abscess can develop rapidly after the inciting event (e.g., trauma) and often include:
- Severe Nasal Obstruction: This is the hallmark symptom. Patients typically experience sudden onset of bilateral (or sometimes initially unilateral) nasal blockage that is progressive and severe, often described as feeling completely "stuffed up." This is due to the hematoma or abscess physically occluding both nasal passages.
- Nasal Pain and Tenderness: The nose, particularly the septum and tip, may be very painful and tender to the touch.
- Swelling of the Nose: External nasal swelling may or may not be present, depending on the nature of any associated trauma. Internal swelling of the septum is characteristic.
- Headache: Often localized to the nasal or frontal region.
- Rhinorrhea: Nasal discharge may be present, initially clear or bloody (with hematoma), and becoming purulent (thick, yellow, or green) if an abscess develops.
If a septal hematoma progresses to an abscess, additional systemic symptoms usually develop:
- Fever and Chills: A rise in body temperature is a strong indicator of infection and suppuration of a hematoma.
- Malaise: A general feeling of illness and discomfort.
- Increased Pain: The nasal pain may become more intense and throbbing.
- Erythema (Redness): The skin over the nose or the nasal mucosa may appear red and inflamed.
On rhinoscopy (examination of the nasal cavity), a septal hematoma appears as a bilateral (or sometimes unilateral if small), smooth, reddish or bluish, fluctuant (boggy or compressible) swelling of the nasal septum, typically in the anterior portion. This swelling can completely close off both nasal passages. A septal abscess will have a similar appearance but may be more erythematous, exquisitely tender, and pus may be visible or aspirated on puncture.
Diagnosis of Nasal Septal Hematoma and Abscess
The diagnosis of nasal septal hematoma and abscess is primarily clinical, based on history and physical examination. Key diagnostic steps include:
- History: Eliciting a history of recent nasal trauma is crucial. The rapid onset of severe bilateral nasal obstruction following trauma is highly suggestive. Inquire about fever, pain, and previous nasal issues.
- Physical Examination (Anterior Rhinoscopy): Visualization of the characteristic bilateral, smooth, fluctuant swelling of the anterior nasal septum is diagnostic. The color may be reddish-purple (hematoma) or more intensely red and inflamed (abscess). Palpation with a cotton-tipped applicator can confirm the soft, compressible nature of the swelling, distinguishing it from a deviated septum or turbinate hypertrophy.
- Needle Aspiration (Puncture): A diagnostic (and often therapeutic) puncture of the septal swelling with a sterile needle and syringe is a key step.
- Aspiration of non-clotted blood confirms a septal hematoma.
- Aspiration of pus (thick, yellowish-green fluid) confirms a septal abscess. The aspirated pus should be sent for Gram stain, culture, and antibiotic sensitivity testing to guide antibiotic therapy.
- Imaging: Imaging studies like CT scans are generally not required for diagnosis if the clinical picture is clear but may be considered in cases of severe trauma to assess for associated facial fractures, or if intracranial complications are suspected.
It is important to differentiate a septal hematoma/abscess from other causes of nasal obstruction, such as severe mucosal swelling from acute rhinitis, large nasal polyps, or acutely deviated septum following trauma (though a deviation is usually firm, not fluctuant).
Treatment of Nasal Septal Hematoma and Abscess
Both nasal septal hematoma and abscess require prompt surgical drainage to prevent complications. The specific approach depends on whether it is a hematoma or an abscess.
Management of Septal Hematoma
- Incision and Drainage (I&D): The hematoma must be drained as soon as possible. This is typically done under local or general anesthesia. A small incision is made in the septal mucosa over the most fluctuant part of the hematoma on one or both sides. The blood clot is evacuated by suction or expression.
- Nasal Packing or Quilting Sutures: After drainage, measures must be taken to prevent re-accumulation of blood. This can involve:
- Anterior nasal packing inserted into both nasal cavities to compress the septal mucosal flaps against the cartilage.
- Placement of through-and-through "quilting" sutures across the septum to coapt the mucosal flaps.
- Insertion of small drains (e.g., Penrose drain pieces or silicone sheeting) for a short period.
- Systemic Antibiotics: Prophylactic systemic antibiotics are usually prescribed to prevent secondary infection and abscess formation, especially if packing is used.
Management of Septal Abscess
- Urgent Incision and Drainage (I&D): This is a surgical emergency. The abscess must be drained immediately to relieve pressure, remove infected material, and restore blood supply to the cartilage. The procedure is similar to hematoma drainage but may require wider incisions to ensure adequate drainage. A vertical incision on one side and a horizontal or staggered incision on the other side have been described to potentially reduce the risk of through-and-through perforation, though complete drainage is paramount.
- Culture and Sensitivity: Pus obtained during drainage should be sent for Gram stain, culture, and antibiotic sensitivity testing.
- Systemic Antibiotics: Broad-spectrum intravenous antibiotics covering common pathogens (especially *Staphylococcus aureus*, including MRSA if prevalent) should be started immediately and then tailored based on culture results.
- Nasal Packing/Drains: Similar to hematoma management, packing or drains are used to keep the drainage site open and prevent re-accumulation of pus. Drains are left in place until purulent drainage ceases.
- Cartilage Debridement: If necrotic (dead) cartilage is found during surgery, it may need to be carefully debrided.
Historically, after aspiration of a hematoma, an antibiotic solution might have been injected into the cavity, but primary drainage and systemic antibiotics are the mainstay now.
Post-Procedure Care
Following drainage of a septal hematoma or abscess:
- Continue systemic antibiotics as prescribed.
- Regular follow-up with an ENT specialist is crucial to monitor healing, remove packing/drains, and manage any complications.
- Nasal saline rinses may be recommended once packing is removed to keep the nasal cavity clean.
- Avoid strenuous activity until cleared by the surgeon.
Potential Complications
If not treated promptly and effectively, nasal septal hematoma and abscess can lead to serious complications:
- Septal Cartilage Necrosis: Prolonged separation of the perichondrium from the cartilage (by hematoma) or direct destruction by infection (in abscess) can lead to cartilage death.
- Saddle Nose Deformity: Loss of septal cartilage support can cause the bridge of the nose to collapse, resulting in a "saddle nose" cosmetic deformity. This is a common and significant long-term complication.
- Septal Perforation: A hole can develop in the nasal septum, leading to crusting, whistling during breathing, and recurrent nosebleeds.
- Spread of Infection:
- Orbital cellulitis or abscess: Infection can spread to the tissues around the eye.
- Cavernous sinus thrombosis: A rare but life-threatening complication involving a blood clot in a major venous sinus at the base of the brain.
- Meningitis or intracranial abscess: Extremely rare but possible if infection spreads to the brain or its coverings.
- Persistent Nasal Obstruction: Due to scarring or recurrent swelling.
- Cosmetic Deformity of the External Nose.
Prompt diagnosis and treatment are essential to minimize these risks.
Differential Diagnosis of Bilateral Nasal Obstruction
When a patient presents with acute bilateral nasal obstruction, especially after trauma, it's important to consider conditions other than septal hematoma/abscess:
| Condition | Key Differentiating Features |
|---|---|
| Nasal Septal Hematoma/Abscess | History of trauma common; bilateral, smooth, fluctuant, reddish/bluish septal swelling; severe obstruction; pain; fever with abscess. Aspiration yields blood or pus. |
| Severe Acute Rhinitis (Viral/Allergic) | Diffuse mucosal swelling, watery or mucoid discharge (may become purulent); often associated with other cold/allergy symptoms (sneezing, itching). Septum itself not typically fluctuant unless coincidentally deviated. |
| Bilateral Nasal Polyposis | Pale, grape-like masses obstructing nasal passages; often associated with chronic rhinosinusitis or allergy; typically more chronic onset. Firm, not fluctuant. |
| Acute Bilateral Turbinate Hypertrophy | Enlargement of inferior turbinates due to inflammation or allergy; mucosa appears boggy. Septum is normal. |
| Nasal Foreign Bodies (Bilateral - rare) | More common in children; often unilateral with foul discharge, but bilateral possible. Obstruction localized. |
| Choanal Atresia (Bilateral - neonatal emergency) | Congenital blockage of posterior nasal apertures; presents with severe respiratory distress in newborns. |
Prevention and When to Seek Urgent Care
Prevention primarily involves avoiding nasal trauma:
- Use protective gear during contact sports.
- Take precautions to prevent falls, especially in children and the elderly.
It is crucial to seek urgent medical attention (preferably from an ENT specialist or in an emergency department) if you suspect a nasal septal hematoma or abscess, especially after nasal injury, and experience:
- Sudden and severe difficulty breathing through both nostrils.
- Significant nasal pain and tenderness.
- Visible swelling inside the nose that blocks the airway.
- Fever accompanying these nasal symptoms.
Timely intervention significantly improves outcomes and reduces the risk of long-term complications.
References
- Ginsburg CM. Nasal septal hematoma. Pediatr Rev. 1998 Apr;19(4):142-3.
- Alshaikh N, Lo S. Nasal septal abscess in children: from diagnosis to management and prevention. Int J Pediatr Otorhinolaryngol. 2011 May;75(5):737-44.
- Cantrell H, Goyle S, Eloy JA, Liu JK. Nasal septal hematoma and abscess. In: Sataloff RT, Johns MM, Costanzo RM, eds. Sataloff's Comprehensive Textbook of Otolaryngology: Head & Neck Surgery - Rhinology. Jaypee Brothers Medical Publishers; 2015.
- Kucik CJ, Clenney T, Phelan_K. Management of acute nasal fractures. Am Fam Physician. 2004 Oct 1;70(7):1315-20. (Context of trauma)
- Karagama YG, Block L, Agada F, et al. Nasal septal abscess: an unusual complication of acute sinusitis. J Laryngol Otol. 2005 Feb;119(2):141-3.
- Dubey SP, Garap JP. Paediatric nasal septal abscess. Int J Pediatr Otorhinolaryngol. 2000 Dec 1;56(2):115-9.
- Blaivas M, Theodoro D, Sierzenski PR. A new diagnostic modality: an_ultrasonographic_application_for_the_evaluation_of_nasal_septal_hematoma. J Ultrasound Med. 2003 Oct;22(10):1083-6.
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis