Chronic rhinitis
Understanding Chronic Catarrhal Rhinitis
Chronic rhinitis encompasses a group of persistent inflammatory conditions affecting the nasal mucosa. It is broadly distinguished into three main types: catarrhal, hypertrophic, and atrophic rhinitis. Each type has distinct etiological factors, clinical presentations, and management strategies.
Etiology and Clinical Features of Chronic Catarrhal Rhinitis
Chronic catarrhal rhinitis, also known as simple chronic rhinitis, is characterized by persistent, low-grade inflammation of the nasal lining. Key etiological (causative) factors include:
- Recurrent Acute Infectious Diseases: Frequent colds, viral URIs, or unresolved acute rhinitis episodes.
- Adenoid Vegetations (Adenoids): Particularly in children, enlarged adenoids can cause chronic nasal obstruction and discharge, leading to secondary inflammation of the nasal mucosa.
- Environmental Factors: Prolonged exposure to cold, dry air, irritants (smoke, pollution, occupational dusts).
- Hereditary Predisposition: A family history of chronic nasal issues may play a role.
- Systemic Diseases: Certain common systemic illnesses or conditions that affect mucosal immunity or vascular tone.
- Deviated Nasal Septum or other anatomical issues: Can disrupt normal airflow and drainage, predisposing to chronic inflammation.
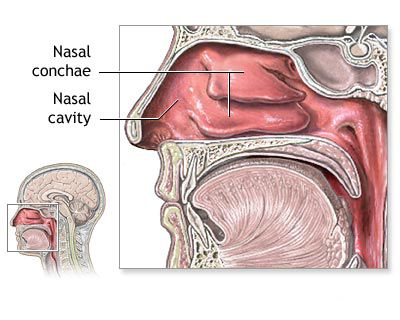
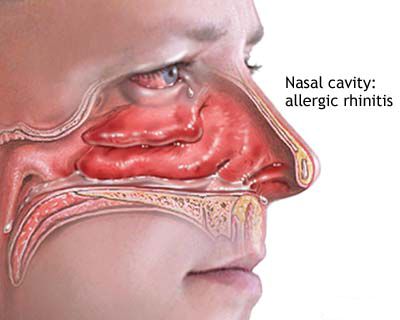
Clinically, chronic catarrhal rhinitis is characterized by diffuse swelling (edema) of the nasal mucosa, which narrows the nasal passages, especially the inferior meatus. Patients typically experience:
- Persistent Nasal Congestion: Often alternating between sides or worsening with changes in position (e.g., lying down).
- Abundant Nasal Secretions (Rhinorrhea): The discharge is usually mucoid or mucopurulent. Normally, the nasal mucosa of a child weighing 10-40 kg produces approximately 300-600 cm3 (or mL) of moisture per day; in chronic catarrhal rhinitis, this volume can exceed 1000 cm3.
- Difficulty with Nasal Breathing: This is a primary complaint.
- Headache: Often dull and related to nasal congestion.
- Potential Complications: Due to impaired drainage and ventilation, complications such as otitis media (middle ear infection), sinusitis (inflammation of paranasal sinuses), and dacryocystitis (inflammation of the lacrimal sac due to nasolacrimal duct obstruction) can arise.
If chronic catarrhal rhinitis has an unfavorable course or is left untreated, it can progress and transform into chronic hypertrophic rhinitis.
Diagnosis and Morphological Changes in Chronic Catarrhal Rhinitis
Differentiating between catarrhal and hypertrophic forms of chronic rhinitis is important for guiding treatment. Diagnostic maneuvers include:
- Adrenaline Test (Anemization): The nasal mucous membrane is lubricated with a 0.1% adrenaline (epinephrine) solution. In chronic catarrhal rhinitis, the swelling of the mucous membrane (particularly of the turbinates) significantly reduces or disappears after application, indicating reversible vasodilation and edema. In hypertrophic rhinitis, the reduction is minimal or absent due to irreversible tissue changes.
- Probe Test (Muck Test - historical): A blunt, bellied probe is gently rubbed over the surface of a turbinate. If an indentation or strip remains, it suggests edematous, boggy mucosa characteristic of the catarrhal form. If no lasting indentation is formed, it points towards the firmer tissue of hypertrophic rhinitis. This test provides an idea of the degree of mucosal swelling and the consistency of the turbinates.
Morphological (histopathological) changes observed in chronic catarrhal rhinitis include:
- Degeneration and a decrease in the number of rows of the ciliated pseudostratified columnar epithelium.
- Exudation of fluid into the tissues.
- Swelling (edema) of the subepithelial layer (lamina propria).
- Vasodilation (enlargement) of blood vessels within the mucous membrane.
- Increased activity of mucous glands.
Treatment and Prevention of Chronic Catarrhal Rhinitis
The primary focus in treating chronic catarrhal rhinitis is to identify and eliminate the underlying etiological factors and to prevent potential complications. Treatment strategies include:
- Addressing Underlying Causes: For example, adenoidectomy if enlarged adenoids are contributing, management of allergies, or avoidance of environmental irritants.
- Topical Medications:
- Astringents: Nasal drops containing 2-3% Protargol (silver proteinate) or Collargol (colloidal silver) may be prescribed for their mild antiseptic and astringent properties.
- Oil-based drops: For older children, peach oil (10 ml) with a small amount of menthol (0.12 ml) can be used as nasal drops for a soothing effect, though menthol should be used cautiously in young children.
- Nasal Saline Irrigation: Regular use of isotonic or hypertonic saline rinses helps to cleanse the nasal passages, remove secretions, and moisturize the mucosa.
- Physiotherapy: If there are no contraindications (such as high blood pressure or certain systemic diseases), various physiotherapy modalities may be employed:
- UHF (Ultra-High Frequency) currents.
- Solux lamp therapy (infrared heat).
- Ultraviolet irradiation (insufflation).
- Microwave therapy.
- Aerosol therapy or negatively charged electroaerosols with antibiotics (after confirming tolerability and if a bacterial component is suspected).
Prevention of chronic catarrhal rhinitis plays a significant role. This includes prompt and adequate treatment of acute respiratory infections, management of allergies, maintaining good nasal hygiene, and promoting overall health through measures like physical training and sports, which can improve general immune function and respiratory health.
Understanding Chronic Hypertrophic Rhinitis
Chronic hypertrophic rhinitis is characterized by a persistent increase in the volume of the nasal turbinates, primarily the inferior turbinates, due to irreversible thickening of the nasal mucosa and sometimes the underlying bone. This hypertrophy leads to significant and often constant nasal obstruction.
Forms and Clinical Manifestations of Chronic Hypertrophic Rhinitis
Chronic hypertrophic rhinitis can manifest in several forms:
- Cavernous or Vascular Form: Dominated by hypertrophy of the erectile vascular tissue within the turbinates. Nasal breathing typically deteriorates with changes in weather conditions, body position (e.g., worsening on the dependent side when lying down), or exposure to irritants. The size of the turbinates significantly reduces after lubrication with a 0.1% adrenaline solution (anemization test is positive).
- Fibrous Form: Characterized by an increase in fibrous connective tissue within the mucosa. In this form, the turbinates are firm, and their size reduces minimally or not at all after adrenaline application (anemization test is negative or weakly positive).
- Papillomatous (Papillary) Form: This is a rare form where the surface of the turbinates, particularly the anterior ends, develops a raspberry-like or mulberry-like appearance due to papillary projections. It causes persistent respiratory failure.
- Osseous (Bony) Form: Involves hypertrophy of the underlying turbinate bone itself, in addition to mucosal thickening.
- Combined Forms: Often, a mixture of these tissue changes is present.
Hypertrophy can be diffuse, affecting the entire turbinate, or localized, commonly affecting the anterior or posterior ends of the turbinates or specific areas on the nasal septum (septal swell bodies, sometimes confused with a prominent Jacobson's organ). Patients with chronic hypertrophic rhinitis typically resort to mouth breathing. They frequently experience associated symptoms such as headaches, sleep disorders, lethargy, and disturbances in the sense of smell (hyposmia or anosmia).
Morphological Changes in Chronic Hypertrophic Rhinitis
Histopathological examination in chronic hypertrophic rhinitis reveals:
- Pronounced proliferation and an increase in the number and size of epithelial cells and mucous glands.
- An increased number of fibroblasts and significant proliferation of connective tissue (fibrosis).
- Thickening of the periosteum and sometimes the underlying bone.
- In the cavernous form, engorgement and hyperplasia of the venous sinusoids (erectile tissue).
Treatment Strategies for Chronic Hypertrophic Rhinitis
The treatment of chronic hypertrophic rhinitis typically requires more active interventions than catarrhal rhinitis due to the irreversible nature of the tissue changes. Medical management with nasal corticosteroids or decongestants may provide some symptomatic relief in milder cavernous forms but is often insufficient for significant fibrous or bony hypertrophy. Therefore, various surgical or procedural measures are employed to reduce turbinate size and improve nasal airflow.
Surgical Techniques: Cauterization, Sclerotherapy, Turbinotomy, Cryotherapy
Common procedural and surgical options include:
- Chemical Cauterization: Application of caustic substances (e.g., trichloroacetic acid, silver nitrate, chromic acid) to the surface of the hypertrophied turbinates. This induces necrosis (tissue death) followed by scarring, which leads to a reduction in turbinate size. However, this method can damage the nasal mucous membrane and destroy the ciliated epithelium, impairing mucociliary function. Its use is now less common.
- Electrocautery (Electroacoustic/Surgical Diathermy): Uses electrical current to cauterize and shrink turbinate tissue. This can be performed superficially or as a submucosal procedure.
- Sclerotherapy (Submucosal Sclerosing Agents): For older children and adults, submucosal injection of sclerosing agents (e.g., 80% glycerol solution, 5% quinine solution, 20% sodium salicylate solution) into the body of the nasal turbinates can induce fibrosis and shrinkage. This technique is less commonly used today due to variable efficacy and potential for complications.
- Turbinoplasty / Turbinotomy (Turbinate Reduction Surgery): These are surgical procedures to reduce the volume of the turbinates. Various techniques exist:
- Submucosal Resection (SMR) of the Turbinate / Submucous Diathermy: The hypertrophied tissue (mucosa, submucosa, or bone) is removed or reduced from beneath the mucosal surface layer, aiming to preserve the overlying ciliated epithelium. Submucosal electrocautery involves inserting a thin needle-like cautery probe into the turbinate parallel to the bone surface; as the hot catheter is slowly withdrawn, it shrinks the tissue. Local anesthesia (e.g., 3-5% cocaine or lidocaine topically, with 0.25-0.5% procaine/novocaine injected) is used.
- Partial Turbinectomy: Excision of a portion of the hypertrophied turbinate, often the anterior or inferior part. For example, with hypertrophy of the anterior end of the inferior turbinate, tissue may be excised in a wedge shape.
- Powered Instrumentation (Microdebrider-Assisted Turbinoplasty): Allows for precise submucosal tissue removal with minimal damage to the surface mucosa.
- Laser Turbinoplasty: Uses laser energy to ablate or shrink turbinate tissue.
- Lateralization of Turbinates: The inferior turbinate bone is fractured at its base and pushed laterally to widen the nasal passage. This is often sufficient to improve nasal breathing and sense of smell.
- Cryotherapy (Cryosurgery): Involves applying extreme cold (e.g., using a liquid nitrogen cryoprobe) to freeze and destroy hypertrophied tissue. This can be done superficially or submucosally. For submucosal cryotherapy, after local anesthesia, a special thin cryoprobe is injected into the turbinate and then slowly removed as it freezes tissue. To protect adjacent structures like the nasal septum, a guard (e.g., of PTFE) may be placed on the cryoprobe or a funnel tube used. Post-procedure, moderate swelling occurs, followed by the formation of a whitish-gray necrotic plaque that sloughs off around the 5th day, revealing a healed surface. Submucosal cryotherapy is suitable for mucosal hypertrophy but not for bony hypertrophy, where submucosal conchotomy or lateralization is more appropriate. For hypertrophy of the posterior ends of turbinates, submucosal cryosurgery is preferred as the surgeon can control probe placement, minimizing risk to the Eustachian tube opening.
The choice of technique depends on the type and extent of hypertrophy, the surgeon's preference, and available equipment. Submucosal techniques are generally favored as they aim to preserve the physiological function of the nasal mucosa and ciliated epithelium, leading to better long-term outcomes with fewer complications like bleeding, adhesions (synechiae), or crusting. Postoperatively, breathing exercises and general physical exercises may be recommended to support respiratory health.
Understanding Chronic Atrophic Rhinitis
Chronic atrophic rhinitis is a debilitating nasal condition characterized by progressive atrophy (shrinkage and thinning) of the nasal mucosa, submucosa, underlying bone (turbinates), and sometimes the nerve supply. It is less common in children than in adults.
Etiology and Symptoms of Chronic Atrophic Rhinitis
The exact etiology of primary atrophic rhinitis (Ozena) is often unclear, but several factors are implicated:
- Environmental Factors: Prolonged exposure to hot, dry, dusty climates or irritants.
- Infections: Chronic bacterial infections, particularly with *Klebsiella ozaenae*, *Proteus vulgaris*, or other specific bacteria, are often associated with Ozena.
- Nutritional Deficiencies: Particularly iron, vitamin A, or vitamin D.
- Endocrine Imbalances.
- Genetic Predisposition: A familial tendency has been observed.
- Autoimmune Processes.
- Iatrogenic Causes (Secondary Atrophic Rhinitis): Can result from previous aggressive nasal surgeries (e.g., excessive turbinate resection leading to "empty nose syndrome"), trauma, or long-term use of certain nasal medications.
Atrophy and subatrophy of the nasal mucosa can occur at any age. The primary symptoms include:
- Nasal Dryness and Itching: A persistent sensation of dryness within the nose.
- Crusting: Formation of thick, often foul-smelling (fetid) crusts that can obstruct the airway. The foul odor is characteristic of Ozena.
- Widened Nasal Passages: Rhinoscopy reveals excessively wide nasal cavities due to atrophy of the turbinates and mucosal lining. The mucosa appears dry, pale, and thin.
- Anosmia or Hyposmia: Loss or significant reduction in the sense of smell, partly due to crusting and damage to olfactory epithelium. Patients themselves may be unaware of the fetid odor due to anosmia (mercy anosmia).
- Epistaxis (Nosebleeds): Due to dryness and friability of the mucosa.
- Sensation of Nasal Obstruction: Paradoxically, despite widened airways, patients may feel obstructed due to altered airflow dynamics and loss of sensory feedback.
Morphological changes are characterized by atrophy of the nasal mucosa with a significant decrease in the number and function of mucous glands and ciliated cells. The ciliated epithelium is often replaced by areas of stratified squamous epithelium (squamous metaplasia). The movement of any remaining cilia is slowed or completely stopped, severely impairing mucociliary clearance.
Treatment Approaches for Chronic Atrophic Rhinitis
Treatment for chronic atrophic rhinitis is primarily symptomatic and aims to keep the nasal passages moist, clear of crusts, reduce odor, and treat any secondary infections. There is no definitive cure for the atrophic process itself. Strategies include:
- Nasal Irrigation and Douching: Regular and frequent irrigation of the nasal cavities with alkaline solutions (e.g., sodium bicarbonate solution) or isotonic/hypertonic saline is crucial to remove crusts, moisturize the mucosa, and reduce odor.
- Topical Lubricants and Moisturizers:
- Application of emollients, oil-based drops (e.g., paraffin oil, sesame oil), or ointments to the nasal mucosa.
- Historically, 1.2% and 5% yellow or white mercury ointment (sometimes mixed with Shostakovskiy balm), or nitrofurazone ointment (1:5000) were used, but mercury-based products are generally avoided now due to toxicity concerns.
- Iodine-Glycerine (Lugol's Solution): Gentle lubrication and massage of the nasal cavity with Lugol's solution (iodine-glycerine) was thought to enhance the function of remaining mucous glands.
- Antibiotics: Topical or systemic antibiotics may be used to treat secondary bacterial infections, often guided by culture of nasal crusts.
- Systemic Medications (Historical/Supportive):
- Potassium iodide solution (e.g., 2% solution, 1/2 teaspoon 2 times a day) was sometimes prescribed.
- Aloe Vera extract injections (up to 30 injections) were explored for their supposed regenerative properties.
- Humidification: Maintaining adequate humidity in the living environment is important to prevent excessive drying of the nasal passages.
- Surgical Procedures (for severe cases to narrow nasal passages):
- Various surgical techniques aim to reduce the size of the nasal cavity to decrease crusting and improve subjective airflow. These include submucosal implants (e.g., cartilage, bone, synthetic materials) into the septum or lateral nasal walls, or partial closure of the nostrils (Young's operation). These are reserved for severe, refractory cases.
If a patient presents with a combination of hypertrophic and atrophic processes in different areas of the nose, treatment must be tailored, addressing hypertrophic areas with reductive methods and atrophic areas with moisturizing and supportive care.
Differential Diagnosis of Chronic Rhinitis Types
Differentiating between the main types of chronic rhinitis is essential for appropriate management:
| Feature | Chronic Catarrhal Rhinitis | Chronic Hypertrophic Rhinitis | Chronic Atrophic Rhinitis (incl. Ozena) |
|---|---|---|---|
| Nasal Mucosa Appearance | Swollen, boggy, often reddish or violaceous; reversible swelling with decongestants. | Thickened, firm, pale or reddish; minimal or no shrinkage with decongestants (especially fibrous/bony forms). May have papillary appearance. | Thin, pale, dry, often covered with crusts. Turbinates appear shrunken. |
| Nasal Passages | Narrowed due to mucosal swelling. | Significantly narrowed or obstructed due to irreversible tissue enlargement. | Excessively wide (roomy). |
| Nasal Discharge | Mucoid or mucopurulent, often abundant. | Variable, can be mucoid or post-nasal drip; less prominent than congestion. | Scanty, thick, forms tenacious crusts. Often foul-smelling (especially in Ozena). |
| Primary Symptom | Nasal congestion, runny nose. | Severe, persistent nasal obstruction. | Nasal dryness, crusting, foul odor (Ozena), sensation of obstruction despite wide passages, anosmia. |
| Response to Decongestants (Anemization) | Good mucosal shrinkage. | Poor or no shrinkage (fibrous/bony forms); some shrinkage in cavernous form. | No effect on mucosal volume; may worsen dryness. |
| Sense of Smell | May be mildly reduced. | Often significantly reduced or absent due to obstruction. | Often absent (anosmia), especially in Ozena. |
| Associated Symptoms | Headache, post-nasal drip. | Headache, mouth breathing, sleep disturbance. | Epistaxis, pharyngitis sicca, laryngitis sicca. |
When to Consult an ENT Specialist
Individuals experiencing persistent nasal symptoms should consult an Ear, Nose, and Throat (ENT) specialist if:
- Nasal congestion, discharge, or obstruction lasts for more than a few weeks despite home care or primary care treatment.
- Symptoms significantly impact quality of life, sleep, or daily activities.
- There is persistent facial pain, pressure, or headache associated with nasal symptoms.
- Recurrent nosebleeds, foul-smelling nasal discharge, or significant loss of smell occurs.
- Over-the-counter medications provide little or no relief.
- There is a suspicion of structural nasal problems or complications.
An ENT specialist can perform a thorough examination, including nasal endoscopy, to accurately diagnose the type of chronic rhinitis and recommend an appropriate, individualized treatment plan, which may include medical therapies, office procedures, or surgical intervention.
References
- Scadding GK, Kariyawasam HH, Scadding G, et al. BSACI guideline for the diagnosis and management of allergic and non-allergic rhinitis (Revised Edition 2017; First edition 2007). Clin Exp Allergy. 2017;47(7):856-889. (General rhinitis context)
- Settipane RA. Rhinitis: A dose of current opinion. Allergy Asthma Proc. 2003;24(3):147-154. (Overview including non-allergic forms)
- Passàli D, Passàli FM, Damiani V, Passàli GC, Bellussi L. Treatment of inferior turbinate hypertrophy: a randomized clinical trial. Ann Otol Rhinol Laryngol. 2003 Sep;112(9 Pt 1):683-8. (Context for hypertrophic rhinitis treatment)
- Hol MKS, Huizing EH. Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniques. Rhinology. 2000 Sep;38(3):157-66. (Review of turbinate surgery)
- Bunnag C, Jareoncharsri P, Tansuriyawong P, Bhothisuwan W, Chantarakul N. Characteristics of atrophic rhinitis in Thai patients at the Siriraj Hospital. Rhinology. 1999 Mar;37(1):29-32. (Specifics on atrophic rhinitis)
- Moore GF, Freeman TJ, Ogren FP, Yonkers AJ. Extended follow-up of patients with atrophic rhinitis treated with rhinoplasty with submucosal Proplast implant. Laryngoscope. 1985 Nov;95(11):1317-9. (Historical treatment context for atrophic rhinitis)
- Mygind N, Dahl R. Anatomy, physiology and function of the nasal cavities in health and disease. Br J Clin Pharmacol. 1998;45(Suppl 1):3S-10S. (General nasal physiology)
See also
Nasal cavity diseases:
- Runny nose, acute rhinitis, rhinopharyngitis
- Allergic rhinitis and sinusitis, vasomotor rhinitis
- Chlamydial and Trichomonas rhinitis
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
- Deviated nasal septum (DNS) and nasal bones deformation
- Nosebleeds (Epistaxis)
- External nose diseases: furunculosis, eczema, sycosis, erysipelas, frostbite
- Gonococcal rhinitis
- Changes of the nasal mucosa in influenza, diphtheria, measles and scarlet fever
- Nasal foreign bodies (NFBs)
- Nasal septal cartilage perichondritis
- Nasal septal hematoma, nasal septal abscess
- Nose injuries
- Ozena (atrophic rhinitis)
- Post-traumatic nasal cavity synechiae and choanal atresia
- Nasal scabs removing
- Rhinitis-like conditions (runny nose) in adolescents and adults
- Rhinogenous neuroses in adolescents and adults
- Smell (olfaction) disorders
- Subatrophic, trophic rhinitis and related pathologies
- Nasal breathing and olfaction (sense of smell) disorders in young children
Paranasal sinuses diseases:
- Acute and chronic frontal sinusitis (frontitis)
- Acute and chronic sphenoid sinusitis (sphenoiditis)
- Acute ethmoiditis (ethmoid sinus inflammation)
- Acute maxillary sinusitis (rhinosinusitis)
- Chronic ethmoid sinusitis (ethmoiditis)
- Chronic maxillary sinusitis (rhinosinusitis)
- Infantile maxillary sinus osteomyelitis
- Nasal polyps
- Paranasal sinuses traumatic injuries
- Rhinogenic orbital and intracranial complications
- Tumors of the nose and paranasal sinuses, sarcoidosis